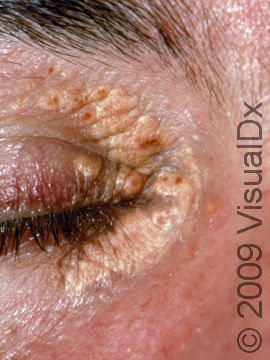
Xanthelasma Palpebrarum
Xanthelasma (xanthelasma palpebrarum) is a skin condition that develops flat yellow growths on the eyelids.
Xanthelasma is often seen in people with high cholesterol or other fat (lipid) levels in the blood, and the lesions contain deposits that are high in fat (lipid-rich).
Who's At Risk?
Xanthelasma can occur in people of any race and of either sex. However, females seem to be more frequently affected than males. In addition, it is unusual for a child or teenager to develop xanthelasma; most individuals develop the condition in middle age.
Approximately one half of patients with xanthelasma have high amounts of fats (lipids) in their blood, such as high cholesterol or high triglycerides.
Signs & Symptoms
The most common locations for xanthelasma include:
- One or both upper eyelids, especially near the nose
- One or both lower eyelids
Xanthelasma appears as a yellow-to-orange patch or bump. Ranging in size from 2–30 mm, xanthelasma is flat-surfaced and has distinct borders (well-defined). Once present, xanthelasma does not usually go away on its own. In fact, lesions frequently grow larger and more numerous.
Xanthelasma is usually not itchy or tender. Individuals with xanthelasma are usually most concerned with their cosmetic appearance.
Self-Care Guidelines
See your doctor for any new skin growth to obtain a correct diagnosis.
Treatments
To confirm your diagnosis of xanthelasma, the doctor may want to perform a skin biopsy. The procedure involves:
- Numbing the skin with an injectable anesthetic.
- Sampling a small piece of skin by using a flexible razor blade, a scalpel, or a tiny cookie cutter (called a “punch biopsy”). If a punch biopsy is taken, a stitch (suture) or two may be placed and will need to be removed 6–14 days later.
- Having the skin sample examined under the microscope by a specially trained physician (dermatopathologist).
Once the diagnosis of xanthelasma is confirmed, the physician will likely check cholesterol levels in your blood (a lipid panel). If you have a lipid abnormality, exercise and dietary modifications will likely be recommended. Many people also require an oral medication to lower their lipids. Treatment of underlying lipid abnormalities does not cure every xanthelasma.
If the xanthelasma is cosmetically unappealing and if it does not respond to lipid-lowering therapies, treatments include:
- Freezing with liquid nitrogen (cryotherapy)
- Surgical excision
- Laser treatment
- Application of a specially formulated acetic acid solution to dissolve the xanthelasma
- Electric needle treatment (electrodesiccation)
All of these treatment options may cause scarring, and they do not keep the xanthelasma from coming back or prevent new lesions from developing.
Visit Urgency
See a dermatologist or another physician if any new growth develops on your skin.
Trusted Links
References
Bolognia, Jean L., ed. Dermatology, pp.1451. New York: Mosby, 2003.
Freedberg, Irwin M., ed. Fitzpatrick’s Dermatology in General Medicine. 6th ed. pp.1467, 1472, 2541. New York: McGraw-Hill, 2003.
Last modified on October 5th, 2022 at 8:10 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder