Tension Headache
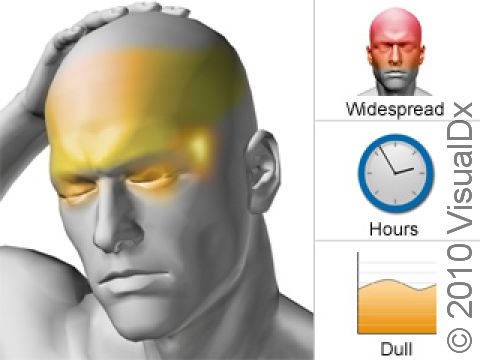
Tension headache involves intermittent episodes of head discomfort that are mild to moderate in intensity, include non-throbbing “tightness” or “pressure,” generally on both sides of the head, and are not aggravated by routine physical activity. Nausea, vomiting, and light/sound sensitivity are rarely present.
Tension headache may last from 30 minutes to 7 days, occurring on more than 1 but fewer than 15 days a month. If headaches are present 15 or more days in a month, the tension headache is considered chronic tension headache (see Chronic Tension Headache topic). People who use pain medications for tension headaches, especially if used regularly, are more prone to developing chronic tension headache. In some cases, not treating the tension headache at all, called undertreatment, can also cause the headache to become chronic tension headache.
Immediately seek medical attention if you or someone you are caring for experiences any of the following:
- Stiff neck and a high fever associated with headache
- Sudden onset of a severe headache
- Loss of motor function, the ability to think clearly, or convulsions associated with headache
- Head injury
- Increased intensity and/or frequency of headaches
Who's At Risk?
Tension-type headache is a little more common in women than men, with onset usually between ages 20 and 30. This type of headache becomes less frequent with age in both sexes. Factors such as fatigue, stress, depression, and anxiety are often present in people with tension headaches. The underlying cause of head pain is thought to involve a “resetting” of the pain threshold in the brain toward greater sensitivity over time.
Signs & Symptoms
This headache syndrome is most notable for its absence of migraine-like features: there is no pulsating sensation, no necessity to lie still in a quiet, dark room. There is generally no history of migraines. People suffering from tension headache often do not stop what they are doing, noting that the headache is a nuisance but not incapacitating. If more severe, headaches can impair concentration, lessen appetite, and make those affected irritable. Tension headache often involves large portions of the head, frequently starting and perhaps staying in the back of the head, neck, and shoulders, with a band-like sensation of pressure in these areas. These regions can also be tender to touch.
Self-Care Guidelines
Many people take non-steroidal medications such as ibuprofen or acetaminophen in an effort to lessen their headaches, which does initially give them the result they are looking for. However, when tension headaches become regular, these medications can contribute to worsening of the headache syndrome. For this reason, if headaches are frequent (ie, 2–3 times a week), generally harmless medications, such as ibuprofen or acetaminophen, should be taken only under guidance by a physician.
Treatments
Simple pain medications are useful for headaches that happen sporadically and may be prescribed in limited amounts by your doctor.
Lifestyle changes are very important in treating tension headaches. The objective is to eliminate influences that precipitate headaches before they become chronic. Well-defined expectations, education, and close consultation with your care provider are essential to success in controlling symptoms. Treatments and strategies that can reduce tension headaches include:
- Physical therapy to work on posture and relax neck, shoulder, and back muscles
- Addressing any anxiety and depression
- Learning how to control frustration/anger through relaxation therapies / hypnosis / biofeedback
- Adjusting physical/lifestyle habits that may be contributing to the headaches (eg, obesity, snoring, diet, poor sleep habits, sedentary lifestyle)
- Dietary monitoring for triggers, elimination of caffeine
- Chronic medication overuse/misuse
- Cognitive-behavioral therapy – talk therapy with a trained counselor, designed to identify stressors and develop coping strategies to minimize their effect on behavior
From a medication standpoint, patients often improve when an overused medication, if present, is effectively eliminated.
Many medications that are effective in treating migraine headaches are utilized to prevent episodic tension headaches that are not frequent enough to be classified as chronic tension headaches. However, the likely impact on the headache is different, and so the medicines that will be tried are in a different order . These medications are taken daily for several months and increased gradually if necessary, with the aim to eventually taper them off.
- The first medications that are usually tried are tricyclic antidepressants (amitriptyline), certain anticonvulsants (gabapentin [Neurontin®], pregabalin [Lyrica®]), and an atypical antidepressant (duloxetine [Cymbalta®]).
- If the first medicines fail, standard migraine-preventative agents such as clonidine, valproic acid, and topiramate may work for some people.
- The ordinary migraine-preventative medicines like beta-blockers (propranolol, atenolol) and calcium channel blockers (verapamil) might be used as a third choice.
- Selective serotonin uptake inhibitors (fluoxetine, sertraline, paroxetine) have been used but make the headache worse for some people.
- Finally, if the approaches above fail, the strategies used in Medication Overuse Headache topic are tried. This involves immediately removing overused medications and quickly starting a single preventative measures listed above along with an oral corticosteroid taper (prednisone or dexamethasone for 3–7 days) or a short course of routine triptan therapy as a “bridge” to relieve headache worsening.
Also prescribed are physical therapy, cognitive behavioral therapy, and referral for counselling/psychotherapy.
Visit Urgency
The majority of tension headaches remain episodic and harmless. However, more serious medical conditions, such as brain tumors and inflammation of blood vessels, can be nondescript and resemble tension headaches. A new headache, one that is significantly different from past headaches, and persistent or changing headaches always require the attention of a doctor.
Contact your doctor in the following situations:
- You develop new symptoms not typical of prior headaches.
- A particularly severe headache occurs.
- Alteration or loss of consciousness occurs.
- Headache persists longer than 3–4 days (unless this is your usual pattern).
- Current therapies/treatments are not working.
- Fever and neck pain or stiffness are present.
- Headache symptoms interfere with activities of daily living (eg, eating, bathing, working, etc).
Over-the-counter medications should be used, on average, only twice a week. Headaches requiring drugs more frequently than this should be brought to your doctors’ attention because overuse of pain medications can facilitate evolution to a chronic headache syndrome. Additionally, if headaches are frequent enough to fulfill previous criteria (see Overview section), you should contact your doctor.
Last modified on October 6th, 2022 at 3:05 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder