Stasis Ulcer
A stasis ulcer is a breakdown of the skin (ulcer) caused by fluid build-up in the skin from poor vein function (venous insufficiency). Fluid leaks from the veins into skin tissue when the blood backs up rather than returning to the heart through the veins.
Who's At Risk?
Leg vein malfunction (venous insufficiency) affects 2–5% of Americans, and approximately half a million Americans have stasis ulcers. Women are more often affected by stasis ulcers than men.
Your risk for acquiring a stasis ulcer is greater if you:
- Are overweight.
- Have varicose veins.
- Have had blood clots in your legs.
- Had a leg injury (trauma) that might affect blood flow in your leg veins; even minor trauma may cause an ulcer.
Signs & Symptoms
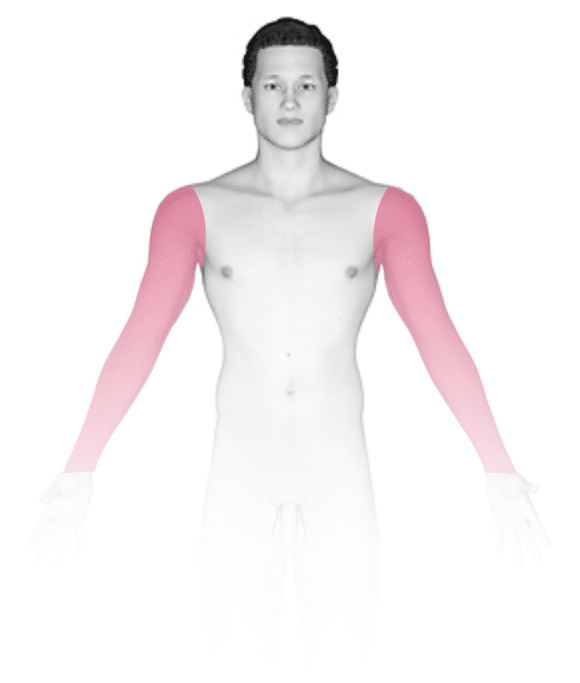
Swelling of the leg, brown discoloration, or an itchy, red, rough area (stasis dermatitis) may appear before you notice an ulcer. This is often seen on the inner ankle area first, although any area on the lower leg may be affected. Varicose veins may be present. Sometimes there are hard, tender lumps under the skin near the ulcer.
The ulcer is a crater-like, irregular area of skin loss. It may be an open, easily bleeding, painful wound, or it might have a thick black scab. The level of pain varies.
Self-Care Guidelines
People with a leg ulcer should seek medical care if it is anything beyond a small scrape or cut on the surface of the skin.
If the ulcer appears minor:
- Clean it with soap and water.
- Apply a thin layer of petroleum jelly (Vaseline®) and a clean gauze bandage.
- Avoid putting any tape or adhesive on the skin.
- Avoid using topical antibiotics and other over-the-counter products, as people with leg ulcers often become allergic to these products.
Treatments
In addition to a thorough exam, your physician may test to evaluate how well your veins are working.
Treatment may consist of:
- Procedures to reduce leg swelling.
- Medication for any dermatitis or infection that is present.
- Special wound dressings.
- Pentoxifylline to aid healing.
- Surgery if other medical treatment fails.
- Compression hose to prevent the ulcer from coming back.
Most ulcers heal within 1–4 months, but about 25% will still be present after a year.
Visit Urgency
If you have pain, swelling, spreading red areas, fever, or any open wound that does not heal after a few days of self-care, seek medical advice.
Trusted Links
References
Bolognia, Jean L., ed. Dermatology, pp.1635. New York: Mosby, 2003.
Freedberg, Irwin M., ed. Fitzpatrick’s Dermatology in General Medicine. 6th ed. pp.21. New York: McGraw-Hill, 2003.
Last modified on October 5th, 2022 at 8:07 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder






