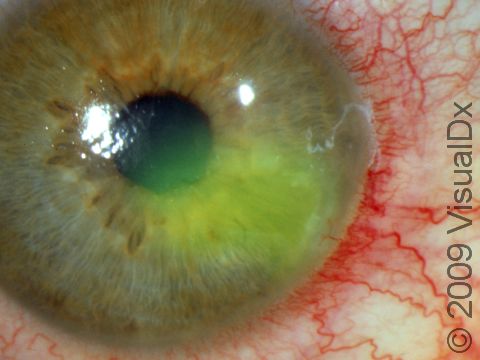
Recurrent Corneal Erosion
Recurrent corneal erosion is the recurrent breakdown of the outermost layer (epithelium) of the cornea. In recurrent corneal erosions, the outermost layer of the cornea fails to glue in tightly to its underlying membrane (basement membrane), making it possible for the epithelium to break off too easily with little effort. There are 3 major causes of recurrent corneal erosion, which are:
- Previous corneal injury (corneal abrasion).
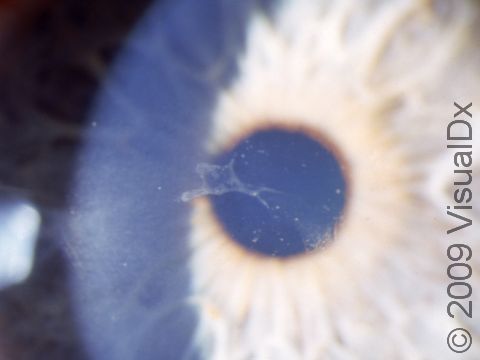
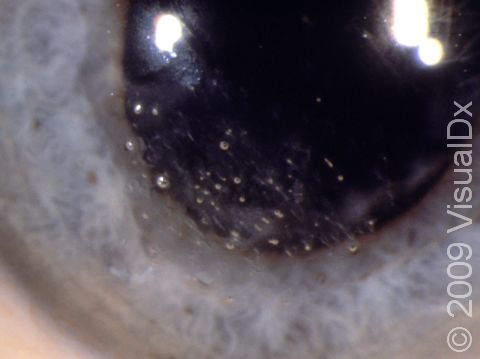
- Corneal dystrophy (map dot fingerprint dystrophy) – (abnormal structure changes of the cornea).
- Underlying corneal disease.
Please see the section on corneal abrasion.
Who's At Risk?
The most likely victim of recurrent corneal erosion is the person who has had a previous corneal abrasion that was very sharp, clean, and linear, like that from a paper cut. Because the cut is so sharp, without ragged edges, it is less likely to stick down tightly to the underlying basement membrane. Think of gluing two pieces of wood together: if they are exceptionally smooth, they might not adhere as well as if the surfaces were rough. Those who have an abnormal structure to the corneal epithelium (called map-dot-fingerprint dystrophy) are at much greater risk of poor healing following a corneal abrasion and, thus, can develop recurrent corneal erosion.
Signs & Symptoms
Just as it is nearly impossible to see a corneal abrasion with the naked eye, the same is true for recurrent corneal erosion. What is most important is the time course. In recurrent corneal erosion, the patient can remember having had a corneal abrasion relatively recently (usually within the past 3–10 days) and then, most often when first opening the eye in the morning, feels a sudden burst of pain accompanied by symptoms of a corneal abrasion, which are:
- Lots of watery tearing
- Sensitivity to light (especially bright light)
- Blurry vision
- Redness of the eye
- Spasm of the muscles surrounding the eye resulting in squinting
- Feeling that something is in the eye
- Pain
Self-Care Guidelines
The self-care for recurrent corneal erosion is very similar to that for corneal abrasions, which is:
- Keep the eye shut.
- Never rub the involved eye at any time (even if it feels fine).
- Immediately remove a contact lens. Contact lens wearers should always have a back-up pair of glasses for when contact lenses shouldn’t be worn.
- Use artificial tears to bathe the eye.
- Use clean water to rinse the eye.
- Use sunglasses to reduce the light sensitivity.
What is very important in self-care is learning how to open your eyes when awakening. The friction of the lid against the sick cornea is enough to rip off a piece of the corneal epithelium, as noted above. So, if you suspect you have recurrent corneal erosion, keep the eye closed firmly and only open the good eye. Look around a little to lubricate the sick eye, so that when you do open it, there is hopefully no friction and, thus, no repeat of the abrasion.
Note:
The good news about recurrent corneal erosion is that, unless there is an ongoing underlying corneal disease, most patients will ultimately heal completely and not have any more episodes. However, it may take years for this to happen.
Treatments
The treatment for recurrent corneal erosion is very similar to that for corneal abrasion. Patching is often very helpful, usually after the instillation of an antibiotic ointment. The doctor may teach you how to open your eye carefully and remind you never to rub the eye. If there is an underlying corneal disease requiring treatment, that too will be addressed. Often, you will be given a salt-like drop for day use and salt-like ointment for nighttime use. The salt pulls fluid out of the corneal epithelium, allowing it to lay down tighter to the underlying basement membrane and, hence, heal better. Map-dot fingerprint dystrophy, which most patients don’t know they have, usually resolves over several years on its own without treatment. Some patients may also be taught how to apply a tight patch that restricts eye movement at night and upon waking so there is less likelihood of recurrence. If these rather simple procedures are not successful, the eye care professional may re-scrape the area to create a more irregular abrasion followed by 1–3 days of patching in hopes of getting the tissues to heal better. Finally, if all this fails to work, the eye care professional may recommend laser treatment to the involved site, called phototherapeutic keratectomy (PTK).
Visit Urgency
Just as noted with corneal abrasions, you should seek medical advice for recurrent corneal erosions when:
- The pain is persisting beyond the first day, or the pain is increasing despite self-care.
- There is no improvement with self-care after 24 hours.
- There is progressive vision loss.
- It is more than once that the abrasion has recurred.
- You develop a mucoid or pus-like discharge from the eye.
Trusted Links
References
Yanoff M, Duker JS, eds. Ophthalmology. 2nd ed, pp. 416-419. St. Louis, MO: Mosby, 2004.
Last modified on October 5th, 2022 at 7:52 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder