Poison Ivy, Oak, and Sumac
Poison ivy, poison oak, and poison sumac dermatides are all an allergic reaction to the oil found on the leaves and in the stems and roots of poison ivy, poison oak, and poison sumac plants (of the Rhus genus). The allergy starts after repeated exposure to the plant and may occur at any age. People usually develop an itchy rash of raised bumps (papules) and blisters in the affected areas.
- Itching can be intense, and scratching may break the skin, resulting in bacterial infection.
- Scratching does not spread lesions. Rather, the lesions with the most exposure appear first, and then, as the allergic reaction (immune response) increases, lesions with less exposure begin to appear.
- Skin lesions usually begin to appear 48 hours after exposure.
Who's At Risk?
Poison ivy, poison oak, and poison sumac may affect people of all ages.
Signs & Symptoms
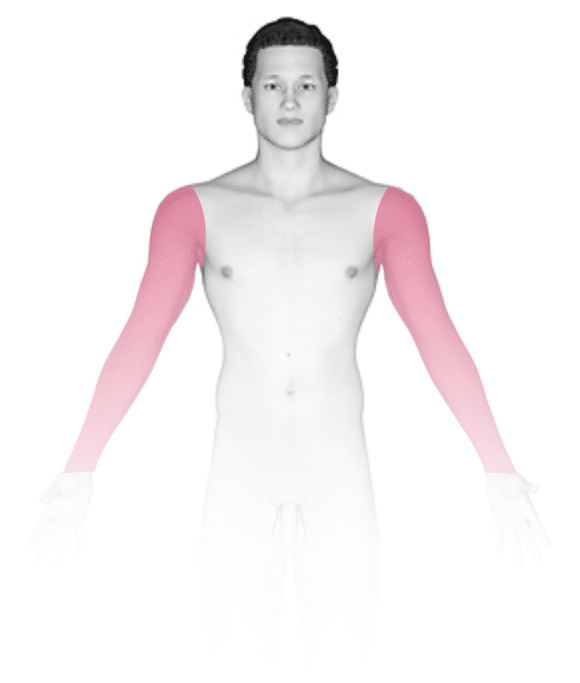
- Poison ivy, poison oak, and poison sumac can occur anywhere on the body where the exposure to the plants has occurred. The arms, legs, face, and neck are commonly affected. Red and brown-red sheets of skin (plaques) and blisters appear in straight lines, and they may form a crust on top.
- In one type of reaction (“black dot variant”), the oil from the plant leaves a black dot on the skin.
- If the face has been exposed, extreme swelling of the face (facial edema) may develop.
Self-Care Guidelines
- After known plant exposure, use soap and warm water to wash all potentially exposed areas within 20 minutes of exposure, to remove the plant oil. Once the oil has been washed off, there is no risk of spreading the condition to other parts of the body.
- Be sure to wash clothes, gloves, and shoes as well.
- Try soothing oatmeal baths (Aveeno® powder) and apply calamine lotion to help relieve symptoms.
- Wear protective clothing and apply barrier cream (Ivy Block™) 15 minutes before potential exposure, to avoid future reactions.
- Try over-the-counter 1% hydrocortisone cream for mild outbreaks.
- Try oral antihistamines (chlorpheniramine or diphenhydramine) to help relieve the itch, but these may cause drowsiness.
- DO NOT USE topical anesthetics containing benzocaine or diphenhydramine, as people easily become allergic to these products.
Treatments
Your physician may prescribe:
- A 14–20 day course of oral prednisone if you have a severe outbreak, affecting large body areas.
- Medium-to-high-potency topical steroids to treat the trunk and arms and legs or low-potency topical steroids to treat the face and skin-fold areas if the affected areas are more limited.
- Oral antihistamines for itching.
- Topical or oral antibiotics if bacterial infection may be present.
Visit Urgency
See your child’s doctor or a dermatologist for evaluation if the rash does not improve with self-care measures or appears to be getting worse.
Trusted Links
References
Bolognia, Jean L., ed. Dermatology, pp.227-229. New York: Mosby, 2003.
Freedberg, Irwin M., ed. Fitzpatrick’s Dermatology in General Medicine. 6th ed, pp.1167-1168. New York: McGraw-Hill, 2003.
Last modified on October 10th, 2022 at 8:28 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder










