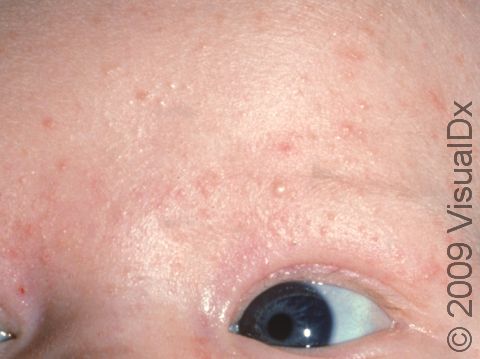
Baby Acne (Neonatal Acne)
Babies can develop blemishes on their face that looks exactly like acne commonly seen in teens. Although the cause of baby acne is unknown, it may be the result of maternal or infant hormones (androgens) stimulating glands in the face to produce oil, or sebum. Baby acne can essentially be divided into 2 groups: neonatal acne, which affects babies in their first month of life; and infantile acne, which typically affects babies 3–16 months of age. Neonatal acne that is confined to the face is called benign cephalic pustulosis, while infantile acne is usually more severe than neonatal acne and consists of more lesions. The later form may last a few weeks to a few months, but most cases usually resolve by age 3.
Who's At Risk?
Neonatal acne occurs in about 20% of newborns. Infantile acne appears to be less common. Males tend to be more affected than females, although this reason is unknown.
Signs & Symptoms
Baby acne consists of multiple red, raised pimples and pus-filled bumps, commonly found on the baby’s face, neck or trunk. Skin can have blackheads and whiteheads present as well. Pitting and scarring of the affected areas can occur in approximately 10–15% of affected infants.
Self-Care Guidelines
In mild cases of baby acne, using a daily cleanser is usually the first step in treatment. Gentle, fragrance-free cleansers are best and should be applied to the affected area daily. Newborns and infants have very sensitive skin, so vigorous scrubbing should be avoided.
Treatments
In mild cases, prescription therapy is generally unnecessary, and the lesions may resolve with gentle cleansing of the skin. The first-line treatment most physicians prescribe is 2.5% benzoyl peroxide. This is an gel that is applied to the skin; it is a commonly used acne product. It is generally well tolerated but may cause dryness. The next line of therapy, in severe cases, is to add an oral antibiotic. Most infants are able to stop oral antibiotics within 18 months. Rarely, cases of acne could be made worse by a fungus, which would require a topical antifungal applied to the skin for treatment. Your baby’s pediatrician may request the help of a pediatric dermatologist for severe cases of acne. Furthermore, in severe cases or those resistant to therapy, an investigation for an underlying hormonal (endocrine) disorder may be warranted.
Visit Urgency
In general, baby acne is harmless and does not require urgent care. If you have any questions or feel that the acne on your baby’s skin is worsening despite using daily cleansing with a gentle soap, it is best to see your pediatrician. Additionally, if your baby is prone to scratching or picking at these lesions, there is a risk the affected areas could develop a bacterial skin infection, and it is best to seek further medical care.
Trusted Links
References
Behrman, Richard E., Robert Kliegman, and Hal B. Jensen. Nelson Textbook of Pediatrics. Elsiever Health Sciences: July 2007.
Habif. Clinical Dermatology, 4th Edition. Mosby Inc: New York, 2004.
Zitelli, Basil J and Holly Davis. Atlas of Pediatric Physical Diagnosis. Mosby Inc: August 2007.
Last modified on October 5th, 2022 at 7:01 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder