Melanoma
Skin cancer is the most common cancer in the United States, and it is the sixth most common cause of cancer death in the United States. Melanoma is the least common of the skin cancers (the other types are squamous cell carcinoma and basal cell carcinoma), but it is the most serious. It can be life threatening if it spreads (metastasizes) to other parts of the body. The frequency of diagnosis of melanoma has been increasing in recent years, faster than any other cancer.
Melanoma starts in the color-producing cells of the skin and may develop in an existing mole or may occur as a new mole. Early diagnosis and treatment can lead to a complete cure, while advanced forms are likely to have a poor outcome. Advanced melanoma can spread to lymph nodes as well as other areas in the body, typically the lungs, liver, and brain.
Who's At Risk?
You have an increased risk of developing melanoma if you have:
- A family history of melanoma – Having someone in your family with melanoma increases your risk tenfold.
- Fair skin, light eyes, and a tendency to freckle – The risk of getting melanoma is 1 in 50 for whites, 1 in 200 for Hispanics, and 1 in 1,000 for people of African descent.
- A large number of moles, especially unusual appearing moles.
- History of frequent sun exposure, especially in childhood.
- History of sunburns.
- Decreased immune system, such as transplant patients and patients with HIV/AIDS.
Melanoma may be seen at any age, but it is most often diagnosed during middle age.
Sunlamps and tanning beds may increase your risk of melanoma, especially if they cause sunburn.
Signs & Symptoms
Melanoma usually occurs on areas of the skin that are exposed to the sun, but it may be found anywhere on the body, including the eye, mouth, and genital area.
- Men are most likely to develop melanoma on the head, neck, and trunk.
- Women are most likely to develop melanoma on the legs and arms.
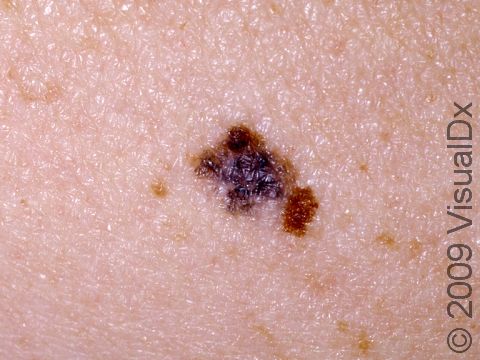
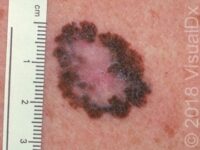
A helpful tool to help you identify a mole that may be melanoma is the ABCDE checklist:
- A – Asymmetry: One half of the mole does not look like the other half.
- B – Border: The outline of the mole is irregular.
- C – Color: More than one color can be seen, such as brown, black, red, blue, and white.
- D – Diameter: A mole larger than 6 mm (1/4 inch), which is roughly the size of a pencil eraser.
- E – Evolving: Changes in the mole over time.
Self-Care Guidelines
Protective measures, such as avoiding skin exposure to sunlight during peak sun hours (10 AM to 3 PM), wearing protective clothing, and applying high-SPF sunscreen, are essential for reducing exposure to harmful ultraviolet (UV) light. These protective measures are especially important in children because 80% of our lifetime exposure to UV light occurs before age 18.
Once a month, you should perform a self-exam to look for signs of skin cancer. It is best to perform the exam in a well-lit area after a shower or bath. Use a full-length mirror with the added assistance of a hand mirror when necessary. Using a hair dryer can help you examine any areas of skin covered by hair, such as your scalp.
- In front of a full-length mirror, inspect the front of your body, making sure to look at the front of your neck, chest (including under breasts), legs, and genitals.
- With your arms raised, inspect both sides of your body, making sure to examine your underarms.
- With your elbows bent, examine the front and back of your arms as well as your elbows, hands, fingers, area between your fingers, and fingernails.
- Inspect the tops and bottoms of your feet, the area between your toes, and toenails.
- With your back to the mirror and holding a hand mirror, inspect the back of your body, including the back of your neck, shoulders, legs, and buttocks.
- Using a hand mirror, examine your scalp and face.
As you perform your monthly self-exam, familiarize yourself with the moles, freckles, and other marks on your body, and look for any changes in them, including shape, size, color, or other changes, such as bleeding or itching.
Treatments
If your doctor thinks that your mole is suspicious for melanoma, you will need a skin biopsy, usually performed by a dermatologist. The goal of the biopsy, also called an excision, is to remove the entire mole and to get a diagnosis.
Prognosis and treatment depend on how deep the tumor has grown into the skin. If you have a melanoma that is very thin (less than 1 mm) and has been completely removed with the excision, this may be all the treatment you need.
For thicker melanomas, your doctor will probably recommend a biopsy of your lymph nodes to determine if they contain melanoma cells. This is called a sentinel node biopsy. If these lymph nodes do have melanoma cells, you may need to have other lymph nodes surgically removed.
If you have lymph nodes that contain melanoma, your doctor will also need to determine if the melanoma has spread to other parts of your body. You may have to have a chest X-ray, a CT scan, an MRI, and/or other tests to determine this.
Treatment for melanoma that has spread to the lymph nodes or other parts of the body may include chemotherapy. For patients with melanoma that has metastasized, immunotherapy is another treatment that can help the body’s own immune system to destroy cancer cells. Types of immunotherapy include vaccines, cytokines (proteins that boost the immune system), and interferon-alpha.
If you have previously been diagnosed and treated for melanoma, you are at increased risk of developing another melanoma, especially in the first 3 years after diagnosis. Therefore, it is essential that you regularly follow up with your doctor to have a thorough skin examination.
Visit Urgency
Use the ABCDE checklist described above to help you decide which moles are concerning for melanoma. If you have a mole that you think fits one or more of these descriptions, call your doctor so he or she can thoroughly examine your skin.
References
American Cancer Society. Detailed Guide: Skin Cancer – Melanoma. http://www.cancer.org/docroot/CRI/CRI_2_3x.asp?rnav=cridg&dt=39. Accessed on January 31, 2009.
Bolognia, Jean L., ed. Dermatology, pp.1789-1815. New York: Mosby, 2003.
Freedberg, Irwin M., ed. Fitzpatrick’s Dermatology in General Medicine. 6th ed, pp.917. New York: McGraw-Hill, 2003.
Ragel EL, Bridgeford EP, Ollila DW. Cutaneous melanoma: update on prevention, screening, diagnosis, and treatment. Am Fam Physician. 2005;72(2):269-276. PMID: 16050450.
Last modified on October 10th, 2022 at 3:11 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder