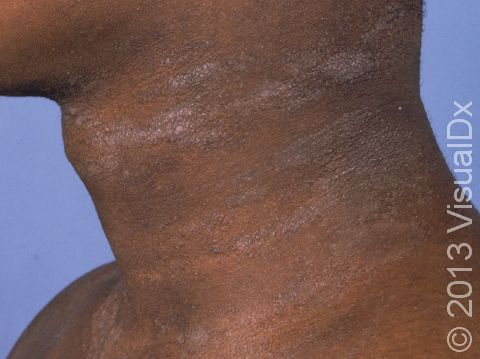
Lichen Simplex Chronicus
Lichen simplex chronicus (LSC), also known as neurodermatitis circumscripta, is an itchy skin condition causing thickened skin at the areas of skin injured by repeated scratching and rubbing.
Lichen simplex chronicus is not a primary disease but rather the skin’s response to chronic physical injury (trauma). The gradual thickening of skin, caused by repetitive scratching and rubbing, is called lichenification.
Lichen simplex chronicus begins as itchy skin. Itching leads to scratching and rubbing, which causes thickening of skin. Thickened skin is itchy, which causes more scratching and, thus, more skin thickening. This scratch-itch cycle then continues if it is not treated.
Who's At Risk?
Lichen simplex chronicus can occur in people of any age, of any race, and of either sex. However, it is more common in females than in males. Though it is rarely seen in children, lichen simplex chronicus can occur in teens and appears more frequently in middle-aged and older adults.
Conditions that can lead to lichen simplex chronicus include:
- Insect bites
- Scars
- Eczema (atopic dermatitis)
- Dry skin (xerosis)
- Poor circulation in the legs (venous insufficiency)
- Anxiety and stress
Signs & Symptoms
Although lichen simplex chronicus can occur anywhere on the body, it is most commonly seen in the following areas:
- Inner wrists, forearms, and elbows
- Sides and back of the neck
- Shins, ankles, and tops of the feet
- Anogenital areas (vulva or scrotum, anus)
Each patch of lichen simplex chronicus appears as leathery, thickened skin in which the normal skin lines are exaggerated. The thickened skin is darker than surrounding skin (hyperpigmented). This hyperpigmentation is even more apparent in darker-skinned individuals.
Individuals with lichen simplex chronicus report periodic itching that is most intense at night and at other times when they are quiet and still.
Self-Care Guidelines
The primary treatment is to stop scratching. However, this can be very difficult once a scratch-itch cycle has started. You may need to cover areas of lichen simplex chronicus at night to keep your child from scratching them during sleep.
Use moisturizers to help relieve itchy skin. When choosing a moisturizer for your child, look for oil-based creams and ointments, which work better than water-based lotions. Apply moisturizers just after bathing the child, while the skin is still moist.
Apply over-the-counter hydrocortisone cream to reduce the itch. Note that if the itching is limited to the groin area, your child may have a fungal infection (jock itch, tinea cruris) rather than lichen simplex chronicus. Do not apply hydrocortisone to the groin area unless recommended by the doctor.
If there are breaks or cracks in your child’s skin, apply an antibiotic ointment to prevent infection.
Treatments
If it is not certain that your child has lichen simplex chronicus, the doctor may perform a skin biopsy to confirm the diagnosis. The procedure involves:
- Numbing the skin with an injectable anesthetic.
- Sampling a small piece of skin by using a flexible razor blade, a scalpel, or a tiny cookie cutter (called a “punch biopsy”). If a punch biopsy is taken, a stitch (suture) or two may be placed and will need to be removed 6–14 days later.
- Having the skin sample examined under the microscope by a specially trained physician (dermatopathologist).
Once you are sure your child has lichen simplex chronicus, it is important to break the scratch-itch cycle. In addition to the above self-care measures, your child’s doctor may recommend one or more of the following treatments to reduce itching and scratching:
- Aggressive moisturizing
- Corticosteroid (cortisone) creams or ointments
- Creams containing salicylic acid or urea to improve penetration of the topical corticosteroid
- Oral anti-histamines, especially for use at bedtime
- Injection of corticosteroid solution directly into the lichen simplex chronicus lesions
- Ultraviolet light therapy
- Doxepin or capsaicin cream
- Topical or oral antibiotics if infection is present
Visit Urgency
See your child’s doctor if the itching does not improve with self-care measures, if more lesions are appearing, or if your child develops symptoms of infection such as pain, redness, drainage of pus, or fever.
References
Bolognia, Jean L., ed. Dermatology, pp.117-118. New York: Mosby, 2003.
Freedberg, Irwin M., ed. Fitzpatrick’s Dermatology in General Medicine. 6th ed, pp.1196-1197. New York: McGraw-Hill, 2003.
Last modified on October 10th, 2022 at 8:38 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder