Scaly Skin (Ichthyosis Vulgaris)
Ichthyosis vulgaris, sometimes known as fish scale disease or common ichthyosis, is a skin disorder in which the skin accumulates much faster than usual, causing thick, dry scales. The scaly skin tends to build up on places where the skin doesn’t rub against itself, so it is usually worse on the legs, arms, and back and less severe on the creases of the groin and armpits. Though the scaly skin itself is usually not life threatening, it is a difficult disorder to live with because it requires daily upkeep (bathing and applying lotions) to keep the scales under control.
There are many kinds of ichthyosis, but ichthyosis vulgaris is the most common. Most types are passed down in families (hereditary) and appear first in childhood, though, very rarely, can be acquired later in life through certain exposures. Ichthyosis is not contagious.
Who's At Risk?
All races and both sexes are affected by ichthyosis vulgaris, though it is much more common in some regions than others; in the United States, 1 in 300 people have the ichthyosis trait, whereas internationally it is less prevalent. With hereditary ichthyosis, typically at least one parent has features of dry, scaly skin. It is an autosomal dominant disorder, meaning that if the parent has the trait (and in this case the disease), each child has a 50% chance of acquiring the trait and inheriting the disease.
Signs & Symptoms
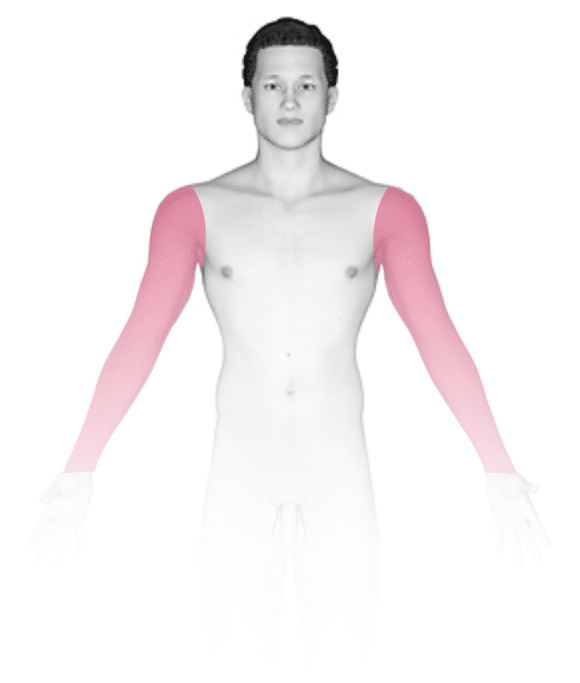
The most common locations for ichthyosis vulgaris include:
- Fronts (extensor surfaces) of the legs
- Backs (extensor surfaces) of the arms
- Scalp
- Back
- Forehead and cheeks, especially in younger children
The scales of ichthyosis vulgaris range in size from 1–10 mm and in color from white to gray to brown, with darker-skinned people often having darker scales. The legs are usually affected more than the arms. The creases on the palms of the hands and the soles of the feet are prominent and often crack during dry or cold weather. However, the scaling tends to improve in more humid or warmer weather.
The following areas tend NOT to be affected:
- Face
- Front of the neck
- Abdomen
- Folds in front of the elbows (flexural surfaces of the arms)
- Folds behind the knees (flexural surfaces of the legs)
Hereditary ichthyosis and acquired ichthyosis look similar, and both are usually itchy. However, the acquired form occurs in people with many internal conditions, including:
- Poor nutrition
- Infections, such as leprosy or HIV/AIDS
- Glandular diseases, such as thyroid or parathyroid problems
- Sarcoidosis
- Cancer, such as lymphoma or multiple myeloma
- Use of certain medications, such as nicotinic acid, cimetidine, and clofazimine
Self-Care Guidelines
Hereditary ichthyosis vulgaris tends to improve after puberty, while acquired ichthyosis vulgaris requires treatment of the underlying medical condition.
However, both conditions should improve by restoring moisture (hydration) to the skin. Creams and ointments are better moisturizers than lotions, and they work best when applied just after bathing, while the skin is still moist. The following over-the-counter products may be helpful:
- Preparations containing alpha-hydroxy acids such as glycolic acid or lactic acid
- Creams containing urea
- Over-the-counter cortisone cream (if the areas are itchy)
Any cracks in the skin should be treated immediately with an over-the-counter topical antibiotic ointment (eg, Polysporin® or bacitracin) in order to prevent an infection.
Treatments
To treat the dry, scaly skin of ichthyosis vulgaris, the physician may recommend a topical cream or lotion containing the following:
- Prescription-strength alpha- or beta-hydroxy acids (glycolic acid, lactic acid, salicylic acid)
- Prescription-strength urea
- A retinoid medication such as tretinoin or tazarotene
- High concentrations of propylene glycol
For more severe, stubborn ichthyosis vulgaris, oral treatments may include:
- Isotretinoin, a very strong medication with many potential side effects, usually used in the treatment of severe, scarring acne
The prognosis for someone with hereditary ichthyosis vulgaris is excellent, as most individuals improve after puberty.
If acquired ichthyosis vulgaris is suspected, the doctor will likely attempt to determine the underlying medical condition or the medication that triggered its development. The prognosis for an adult with acquired ichthyosis vulgaris depends upon treating the underlying medical condition or discontinuing the triggering medication.
Visit Urgency
If you have very dry, scaly skin despite twice daily application of an over-the-counter moisturizer, be sure to tell your doctor.
References
Bolognia, Jean L., ed. Dermatology, pp.775-781. New York: Mosby, 2003.
Freedberg, Irwin M., ed. Fitzpatrick’s Dermatology in General Medicine. 6th ed, pp.486, 482, 2353. New York: McGraw-Hill, 2003.
Last modified on August 16th, 2022 at 2:44 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder






