Herpetic Whitlow
Herpetic whitlow, also called digital herpes simplex, finger herpes, or hand herpes, is a painful viral infection occurring on the fingers or around the fingernails. Herpetic whitlow is caused by infection with the herpes simplex virus (HSV).
Infections with HSV are very contagious and are easily spread by direct contact with infected skin lesions. HSV infection usually appears as a group of small vesicles (fluid-filled blisters), erosions (sore areas of missing skin), or crusts (scabs) around the mouth, nose, genitals, and buttocks, but infections can develop almost anywhere on the skin. Furthermore, these tender sores may recur periodically in the same sites.
There are 2 types of HSV: herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2). Infections around the mouth, lips, nose, or face are usually caused by HSV-1. HSV-2 more commonly causes lesions on the genital area. Both conditions can occur on virtually any body location.
Both types of HSV produce 2 kinds of infections: primary and recurrent. The sores of a primary infection last about 2-4 weeks. These sores heal completely, rarely leaving a scar. Affected individuals carry the virus in their bodies for the rest of their lives.
Certain triggers can cause the hibernating (latent) virus to wake up, become active, and travel back to the skin. These recurrent HSV infections may develop frequently (every few weeks), or they may never develop. Recurrent infections tend to be milder than primary infections and generally occur in the same location as the primary infection.
People can develop herpetic whitlow when they come into contact with areas already infected with HSV, either on their own bodies or on someone else’s body. Usually, there is a break in the skin, especially a torn cuticle at the base of the fingernail, which allows the virus to enter the finger tissue and establish an infection. Both HSV-1 and HSV-2 can cause herpetic whitlow infections.
Who's At Risk?
Herpetic whitlow can affect people of any age, race / ethnicity, and sex. However, it is more common in children and in dental and medical workers. Children often contract herpetic whitlow as a result of thumb- or finger-sucking when they have a herpes infection of the lips or mouth. Dental and medical workers may contract herpetic whitlow by touching the contagious lesions of a patient with HSV infection. In these groups of people—children and health care workers—herpetic whitlow is most commonly caused by HSV-1. In others, herpetic whitlow is usually caused by infection with HSV-2.
Signs & Symptoms
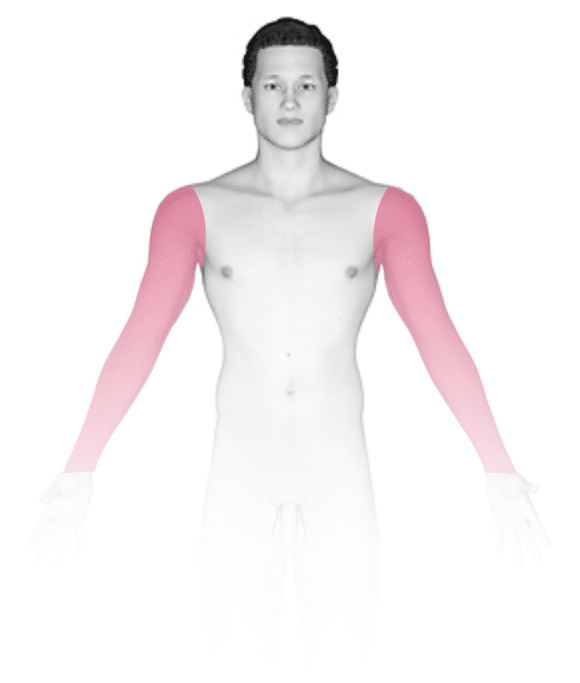
The most common locations for herpetic whitlow include the:
- Thumb.
- Index finger.
- Other fingers.
Approximately 5-7 days after the initial exposure to HSV, the infected area develops burning, tingling, and pain. Over the next week or 2, the finger becomes inflamed and swollen. Small (1-3 mm) vesicles (fluid-filled blisters) develop, often clustered together on a bright red or darker-than-normal skin color (hyperpigmented) base. The vesicles usually rupture and scab over, leading to complete healing after an additional 2 weeks.
Other symptoms occasionally associated with the primary infection of herpetic whitlow include:
- Fever.
- Red streaks radiating from the finger (lymphangitis).
- Swollen lymph nodes in the elbow or underarm area.
Coexisting herpes simplex virus infection of the mouth area or of the genital area may also be present.
Recurrent HSV infections are often milder than the primary infection, although they look similar. A recurrent infection typically lasts 5-10 days. Recurrent herpetic whitlow is rare.
People with recurrent HSV infections may report that the skin lesions are preceded by sensations of burning, itching, or tingling (prodrome). About 24 hours after the prodrome symptoms begin, the actual lesions appear as one or more small blisters, which eventually open up and become scabbed over.
Self-Care Guidelines
Acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) may help reduce fever and pain caused by the herpes sores. Applying cool compresses or ice packs may also relieve some of the swelling and discomfort.
Because HSV infections are very contagious, it is important to take the following steps toward preventing spread (transmission) of the virus during the prodrome phase (burning, tingling, or itching) and active phase (presence of blisters or sores) of herpetic whitlow:
- Avoid sharing towels and other personal care items.
- Cover the affected finger with a bandage.
- Wear gloves if you are a health care provider.
- Avoid popping any blisters, as it may make the condition worse.
Unfortunately, the virus can still be transmitted even when someone does not have active lesions. However, this is uncommon for people with herpetic whitlow.
Treatments
Most HSV infections are easy for medical professionals to diagnose. On occasion, however, a swab from the infected skin may be sent to the laboratory for viral culture, which takes a few days to grow. Blood tests may also be performed.
Untreated HSV infections will go away on their own, but medications can reduce the symptoms and shorten the duration of outbreaks. There is no cure for HSV infection.
Although herpetic whitlow symptoms will eventually go away on their own, your medical professional may prescribe antiviral medications to help relieve symptoms and prevent spread of the infection to other people, such as acyclovir (Zovirax), valacyclovir (Valtrex), or famciclovir (Famvir).
More severe herpetic whitlow may require oral antibiotic pills if the area is also infected with bacteria.
Visit Urgency
If you develop a tender, painful sore on the finger, see a medical professional, especially if it is not going away or if it seems to be getting worse. Seek medical attention right away if you have a finger sore as well as typical symptoms of oral or genital herpes.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on April 3rd, 2023 at 10:34 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder





