Folliculitis
Folliculitis is a skin condition caused by inflammation of the hair follicles. It usually occurs in areas where the skin is irritated by friction, such as rubbing from clothes. In most instances of folliculitis, the inflamed follicles are infected with bacteria, especially the type called Staphylococcus (or “staph”), that normally live on the skin. Bacteria such as Pseudomonas may live in hot tubs, spas, and swimming pools and may also cause folliculitis.
Who's At Risk?
Folliculitis occurs in people of all ages, races / ethnicities, and sexes. It is very common in children.
Risk for folliculitis is increased by:
- Skin conditions such as eczema, acne, or another dermatitis.
- Excessive sweating.
- Living in a warm, humid climate.
- Diabetes.
- Obesity.
- A weakened immune system due to organ transplantation, cancer, or HIV/AIDS.
- Frequent shaving.
Signs & Symptoms
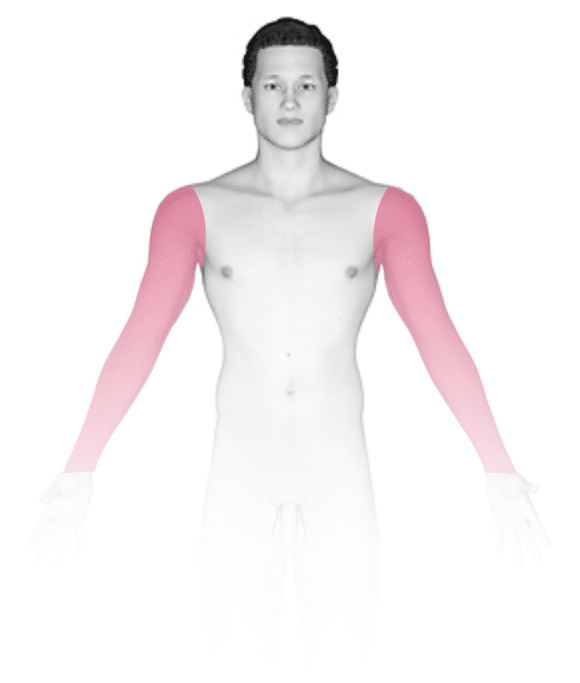
The most common locations for folliculitis in children include the:
- Scalp.
- Face.
- Buttocks.
- Arms and legs.
Individual lesions of folliculitis include pustules (pus-filled bumps) and papules (small solid bumps) centered on hair follicles. These pustules and papules may be pierced by an ingrown hair, can vary in size from 2-5 mm, and are often surrounded by a ring of inflamed skin. In lighter skin colors, the lesions may be any shade of pink or red. In darker skin colors, the redness may be harder to see, and the bumps may be the only sign of the folliculitis. Occasionally, a folliculitis lesion can break open, drain, and form a scab on the surface of the skin.
Both mild and moderate folliculitis are often tender or itchy. More severe folliculitis, which may be deeper and may affect the entire hair follicle, can be painful.
Mild and moderate folliculitis usually go away quickly with treatment and leave no scars. More severe folliculitis may lead to more serious complications, such as an infection of the deeper skin tissue (called cellulitis), scarring, and permanent hair loss in the affected area.
Self-Care Guidelines
To prevent folliculitis, have your child try:
- Avoiding tight clothing, especially during exercise.
- Washing athletic clothing after each use.
To help clear up mild folliculitis, have your child:
- Use an antibacterial wash (eg, PanOxyl Acne Creamy Wash, Hibiclens).
- Apply hot, moist compresses to the affected area.
- Use an over-the-counter corticosteroid cream (hydrocortisone) to help soothe irritated or itchy skin.
- Wash towels, washcloths, and bed linens often.
- Wear loose-fitting clothes.
Treatments
Folliculitis is usually fairly easy to diagnose. Your child’s medical professional may perform a bacterial culture and may recommend:
- Prescription-strength antibacterial wash such as hexachlorophene (eg, pHisoDerm, pHisoHex).
- Topical antibiotic lotion or gel such as clindamycin (eg, Cleocin T).
- Oral antibiotic pills or syrups such as cephalexin (eg, Keflex), dicloxacillin (eg, Vibramycin, Monodox), trimethoprim-sulfamethoxazole (eg, Bactrim), or clindamycin (eg, Cleocin).
If your child’s medical professional prescribes antibiotics, be sure they take the full course of treatment.
Visit Urgency
See your child’s pediatrician, dermatologist, or another medical professional if self-care measures do not heal the condition within 2 or 3 days, if symptoms keep coming back, or if the infection spreads to larger areas or appears somewhere else on the body.
Tell your child’s medical professional about any recent exposure to hot tubs, spas, and swimming pools because a less common form of folliculitis may be caused by bacteria living in these water sources.
If your child is currently being treated for a skin infection that has not improved after 2-3 days of antibiotics, return to the medical professional.
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Paller A, Mancini A. Paller and Mancini: Hurwitz Clinical Pediatric Dermatology. 6th ed. St. Louis, MO: Elsevier; 2022.
Last modified on March 10th, 2023 at 3:56 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder






