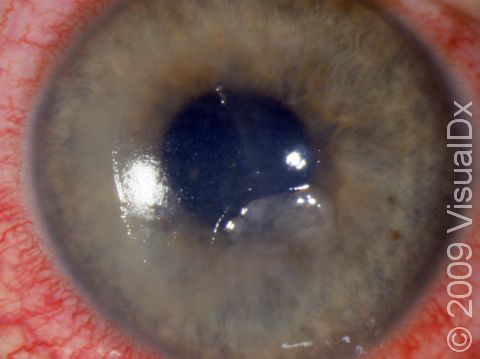
Corneal Abrasion
A corneal abrasion is a scratch or cut (abrasion) of the clear outer layer (cornea) of the eye. Injury (trauma) is the most common cause for corneal abrasions. The most common trauma causes are:
- Scratches from fingernails (human and animal).
- Foreign objects hitting the cornea (eg, dirt, wood splinters, metal shavings, plants, tree branches, etc).
- Curling irons.
- Excessive rubbing of the eye.
- Overexposure to ultraviolet light.
- Arc welding light exposure.
- Over wearing of contact lenses.
- Ill-fitting contact lenses.
- Torn contact lenses.
- Makeup brushes.
- Paper cuts.
- Chemical burns.
- Irregular eyelashes rubbing the cornea or falling off into the eye.
- A foreign object that gets caught under the eyelid, which then irritates the cornea each time you blink.
Other causes include underlying eye conditions, such as:
- Inability to fully close the eyelids.
- Abnormalities of the lid position.
- Severe dry eye conditions.
- Severe, chronic blepharitis (inflamed eyelids).
Who's At Risk?
Corneal abrasions are fairly common. Those who wear contact lenses or work in dusty, dirty, windy, or debris-laden areas are more likely to get a corneal abrasion.
Signs & Symptoms
Although it is very difficult to see a corneal abrasion with the naked eye, you have to be suspicious of this if you have experienced any of the causes of trauma mentioned above. Along with that is the unrelenting painful feeling that something is in your eye that just won’t wash out, plus:
- Lots of watery tearing.
- Sensitivity to light (especially bright light).
- Blurry vision.
- Redness of the eye.
- Spasm of the muscles surrounding the eye resulting in squinting.
Self-Care Guidelines
Most simple corneal abrasions will heal on their own within a day or two at most. Other things that help include:
- Keeping the eye shut.
- Never rubbing the injured eye.
- Immediately removing a contact lens. Contact lens wearers should always have a back-up pair of glasses for when contact lenses shouldn’t be worn.
- Using artificial tears to bathe the eye.
- Using clean water to rinse the eye and wash out suspect foreign matter.
- Using sunglasses to reduce light sensitivity.
There are precautions that you can take to prevent getting a corneal abrasion. These include:
- Wearing protective eyewear for all conditions that might result in a corneal abrasion, such as working around the garden, working on grinding machines, etc.
- Being extra careful when using makeup brushes and curling irons.
- Taking excellent care of and using excellent hygiene with contact lenses.
- Never sleeping in contact lenses, regardless of manufacture notes.
Note:
If the corneal abrasion heals and then suddenly recurs days later, this may be a sign of recurrent erosion, which requires specific medical care by an eye care professional. Use of topical anesthetic solutions is only for purposes of diagnosis. Using these drops more than once or twice is dangerous because it slows healing and could lead to more serious conditions.
Treatments
After assurance that there is nothing more serious than an abrasion, your doctor will check for any foreign objects and, if needed, clean the area. Numbing eye drops or oral pain medication may be given. Topical antibiotics also may be used. Patching is no longer recommended because it could delay healing. If there is an underlying basis for the abrasion, care for this is needed to prevent recurrence. If the abrasion was contact-lens–related, you may be required to be reevaluated regarding your contact lenses as to fit and type. If the problem is recurrent erosion, your doctor will begin specific treatment for that condition.
Visit Urgency
- Persistent pain beyond the first day or pain that is increasing despite self-care.
- You suspect that a piece of metal, wood, or plant material hit the eye with high speed and may have penetrated the eye, not just irritated it.
- Any abrasion caused by chemicals, heat burn, makeup brushes, or plant materials.
- You suspect that a foreign object really is stuck in your eye.
- Recurrence of the pain and other symptoms days after the initial injury.
- Mucoid or pus-like discharge.
- No improvement with self-care after 24 hours.
- Progressive vision loss.
Trusted Links
References
Yanoff M, Duker JS, eds. Ophthalmology. 2nd ed, pp. 415-416. St. Louis, MO: Mosby, 2004.
Last modified on October 10th, 2022 at 3:38 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder