Cluster Headache
Cluster headache is considered a primary headache syndrome, one of a group of headaches with distinctly different features compared to other common headache syndromes (eg, tension headache and migraine). The hallmarks of cluster headaches are their occurrence in clusters with quiet periods between clusters and their severity.
Immediately seek medical attention if you or someone you are caring for experiences any of the following:
- Stiff neck and a high fever associated with headache
- Sudden onset of a severe headache
- Loss of motor function, the ability to think clearly, or convulsions associated with headache
- Head injury
- Increased intensity and/or frequency of headaches
Who's At Risk?
Cluster headache is more common in men. People with cluster headache are also more likely to have had stomach ulcers and head injury. The great majority of cluster headache sufferers are smokers, and many have used alcohol for long periods of time.
Signs & Symptoms
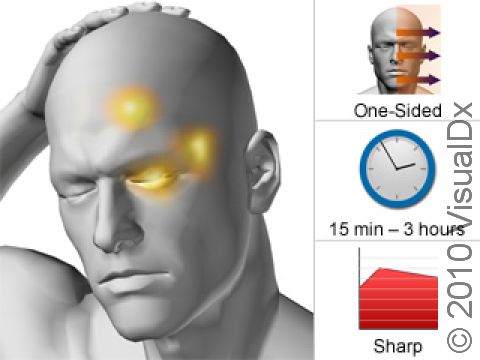
Cluster headache involves frequent attacks of severe, short-lasting, one-sided head pain. The pain is usually most intense behind or around the eye, but it is sometimes reported in the back of the head. Sometimes the pain will shift sides between attacks. Other symptoms that are prominent include tears from that eye (most common), reddening of the eyes, stuffy nose, runny nose, a small pupil on the side of the headache, and drooping of the eyelid on that side. People may be very sensitive to light and sound with cluster headache.
Pain attacks characteristically come in “clusters,” in which groups of headaches last from 15 minutes to 3 hours. Three out of four of all cluster headaches last under an hour. The headaches take place 1–3 times a day. A cluster period, or cycle, is a period of time during which a person is having daily cluster headaches. Cluster cycles generally last from 2–12 weeks, with most patients having 1–2 cluster cycles per year. Most patients are symptom-free between cycles. These asymptomatic periods generally last 6 months to 2 years before a cluster period recurs.
Remarkably, cluster cycles can occur at the same time of year for consecutive years for an individual, and daily cluster headaches have a tendency to occur at specific times of the day. Headaches are particularly common between 1:00–2:00 AM, 1:00–3:00 PM, and after 9:00 PM. Cluster headaches also have a tendency to occur during the first period of very deep REM sleep, such that people awaken with a severe headache 60–90 minutes after going to sleep.
Cluster headache is always severe. While migraine sufferers prefer to lie still in dark, quiet rooms, those who suffer from cluster headaches may writhe or scream in pain, strike walls or other objects with their heads, and find it extremely difficult to sit still.
Self-Care Guidelines
Common pain relief medications, such as ibuprofen and acetaminophen, are not effective for cluster headache. Keeping a headache diary, looking for possible triggers for the clusters, and taking part in stress reduction or relaxation training are all reasonable self-care activities.
Treatments
Three types of treatment are used:
- Medications meant to stop a headache, known as abortive medications, that has recently started.
- Preventative medications, meant to reduce the likelihood of additional headaches within a cluster period.
- Transitional therapy, to lessen symptoms while preventative medications are gaining efficacy.
The best abortive medication is subcutaneous sumatriptan, a drug often used for termination of migraine headaches. Inhaled sumatriptan is also effective, but it is less so than the form injected under the skin. Oral zolmitriptan, another member of this medicine class, can be used for people who cannot tolerate injection. Inhaled 100% pure oxygen will reliably terminate a cluster attack, although some people find the headache will start again once the oxygen is stopped. Oxygen is very favorable because it can be used numerous times daily for weeks at a time without side effects. This is in contrast to the triptans (above), which may result in chronic headache with repetitive use even over short periods of time. Older agents such as ergot derivatives have also proven useful to stop cluster headaches.
Preventative medications include verapamil, a medication also used for migraines and high blood pressure, lithium (often used for mood stabilization), valproic acid or topiramate (both used for seizures), and melatonin. These drugs are used only during a cluster cycle and are tapered off when a cluster period seems to be over. There is no evidence that taking these agents continuously between cluster cycles will prevent onset of future cycles.
In some cases, much higher doses of these medications are necessary in comparison to their use for other medical conditions. Ask your doctor to review the dose-dependent side effects if escalating doses are necessary. For example, doses of verapamil above 480 milligrams require EKG (electrocardiogram) monitoring of the heart with each change in dosing. This is to assess for possibly excessive interference with the electrical conduction of the heart. Furthermore, more than one preventative medication may be necessary to get attacks under control.
Because it may take weeks for preventative medications to achieve sufficient blood levels, corticosteroids, ergot derivatives given intravenously (eg, dihydroergotamine), longer-lasting triptans (eg, naratriptan), and nerve blockade (ie, injection of anesthetic and steroid into a nerve near the base of the skull) can be used to relive symptoms in the interim. These medications are given for 7–14 days while a preventative medication is being instituted and titrated to appropriate doses.
Rarely, surgical treatments are prescribed if medical options have been exhausted. These techniques involve damage to nerves that supply sensation to the face and less commonly the nerves that precipitate watery eyes / runny nose / congestion symptoms. While some patients are pain free for long periods of time, return of pain, painful numbness, and extensive numbness of the face and eye are all possible. Newer techniques are experimenting with electrode implantation in a deep part of the brain, the hypothalamus, a location that might initiate or modulate the regularity of the attacks. These options will be discussed by your doctor only after extensive medication trials are undertaken.
Visit Urgency
All cluster headaches require treatment. Cluster headache is frequently misdiagnosed as migraine because of the one-sided head pain and frequent light and sound sensitivity. If you suspect your headaches have additional features similar to the above description, contact your doctor.
Always contact your doctor in the following situations:
- You develop new symptoms not typical of prior headaches.
- A particularly severe headache occurs.
- Alteration or loss of consciousness occurs.
- Headache persists longer than 3–4 days.
- Current therapies/treatments are not working.
- Fever and neck pain or stiffness are present.
- Headache symptoms interfere with activities of daily living (eg, eating, bathing, working, etc).
Last modified on October 6th, 2022 at 3:05 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder