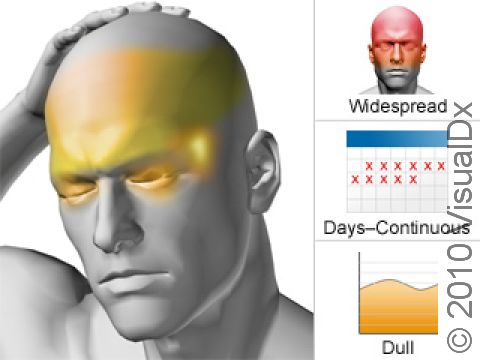
Chronic Tension Headache
Chronic tension headache is a syndrome of headaches that are mild to moderate in intensity, involve “tightness” or “pressure” on both sides of the head, and are not aggravated by routine physical activity. Nausea, vomiting, and light/sound sensitivity are usually not present and, if so, are mild and infrequent. The headache most often starts in the back of the head or neck, although it can start anywhere, and moves to include the whole head. It may worsen as the day goes on. Headaches of this description must be present for 15 or more days of a month for at least 3 months. When more severe, the headache can be continuous. Chronic tension headache often evolves from episodic tension headache, which is very similar in description but far less frequent.
Immediately seek medical attention if you or someone you are caring for experiences any of the following:
- Stiff neck and a high fever associated with headache
- Sudden onset of a severe headache
- Loss of motor function, the ability to think clearly, or convulsions associated with headache
- Head injury
- Increased intensity and/or frequency of headaches
Who's At Risk?
Chronic tension-type headache affects women more than men and becomes more frequent with age in both sexes. People who use pain medications for treating episodes of tension headaches are more prone to developing chronic tension headache. Factors such as fatigue, stress, depression, and anxiety are often present in people with chronic tension headaches. The underlying cause of head pain is thought to involve a “resetting” of the pain threshold in the brain toward greater sensitivity over time.
Signs & Symptoms
Chronic tension headache is most notable for its absence of migraine-like features; there is no pulsating sensation and no necessity to lie still in a quiet, dark room. The person suffering from chronic tension headache generally has no history of migraines. Additionally, chronic tension headache does not typically cause the sufferer to stop what he/she is doing, noting that the headache is a nuisance but not incapacitating. It often involves large portions of the head, frequently the back of the head and neck, and involves a band-like sensation of pressure in these areas. These areas can also be tender to touch.
Self-Care Guidelines
Many chronic tension headache sufferers take over-the-counter pain relievers such as ibuprofen, naproxen, or acetaminophen in an effort to lessen their headaches. These medicines seem to work well when the headaches first start, but when tension headaches become daily, they can contribute to worsening of the headache syndrome (see Medication Overuse Headache). For this reason, if headaches are frequent (ie, 2–3 times a week), even seemingly safe medicines, such as those mentioned above, should be taken only after discussing them with your doctor.
Other approaches to headache management that you can try include reduction of stress, relaxation training, and biofeedback. Massage can also be effective. Avoiding poor posture, practicing proper computer use, and limiting eye strain are all also important.
Treatments
As one of the chronic daily headache syndromes, the treatment of chronic tension headache is similar to that of chronic migraine.
Chronic tension headache is often present for years by the time a comprehensive treatment plan is created for a particular person that is effective. Many possible influences are interwoven in the regimens/lifestyles that maintain chronic tension headaches. In chronic tension headache, a variety of contributing factors must be addressed:
- Anxiety and depression
- Frustration
- Physical and emotional dependence
- Physical/lifestyle factors that may exist (eg, obesity, snoring, diet, poor sleep habits)
- Chronic medication overuse/misuse
Well-defined expectations, education, and close follow-up are essential to success in controlling symptoms. What is particularly challenging for sufferers of chronic tension headache and their physicians is that headache often worsens with treatment and lifestyle interventions before it improves. Strategies employ management of physical/lifestyle factors that may be complicating the headaches while medication detoxification, if applicable, is ongoing. Possibilities include:
- Relaxation therapies / hypnosis / biofeedback
- Dietary monitoring for triggers and elimination of caffeine
- Improving sleep habits
- Daily exercise
- Cognitive-behavioral therapy – This is talk therapy with a trained counselor, designed to identify stressors and develop coping strategies to minimize their effect on behavior.
- Counseling and treatment for depression and/or anxiety
Many medications that are effective for migraine are utilized to provide relief for chronic tension headache. However, the likely impact on the headache is different, and so the medicines that will be tried are in a different order.
- The first medications that are usually tried are tricyclic antidepressants (amitriptyline), certain anticonvulsants (gabapentin [Neurontin®], pregabalin [Lyrica®]), and an atypical antidepressant (duloxetine [Cymbalta®]).
- If the first medicines fail, standard migraine-preventative agents such as clonidine, valproic acid, and topiramate may work for some people.
- The ordinary migraine-preventative medicines like beta-blockers (propranolol, atenolol) and calcium channel blockers (verapamil) might be used as a third choice.
- Selective serotonin uptake inhibitors (fluoxetine, sertraline, paroxetine) have been used but make the headache worse for some people.
- Finally, if the approaches above fail, the strategies used in Medication Overuse Headache topic are tried. This involves immediately removing overused medications and quickly starting a single preventative measures listed above along with an oral corticosteroid taper (prednisone or dexamethasone for 3–7 days) or a short course of routine triptan therapy as a “bridge” to relieve headache worsening.
Also prescribed are physical therapy, cognitive behavioral therapy, and referral for counselling/psychotherapy.
Visit Urgency
You should call your doctor for any headache if:
- You develop new symptoms not typical of prior headaches.
- An unusually severe headache occurs.
- You pass out or lose time.
- Your headache lasts an unusually long time.
- Headache awakens you from sleep
- Fever and neck pain or stiffness are present.
In the case chronic tension headache, you should call your doctor if:
- The headache worsens or the quality of it changes significantly as you try to use the treatments that your doctor recommends.
- You develop side effects from any of the new medications that your doctor suggests to break the chronic headache cycle.
Last modified on October 6th, 2022 at 3:05 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder