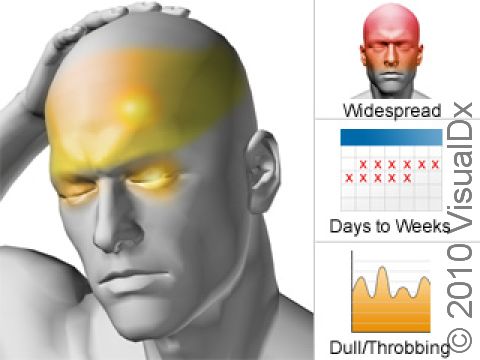
Chronic Migraine
Chronic migraine is defined as daily or nearly daily headaches 15 or more days per month for more than 3 months. It is also called transformed migraine or chronic daily headache by some. Additionally:
- The affected person has suffered at least 5 prior migraine attacks.
- Daily or almost daily headaches that resemble tension-type headaches develop that include pain on both sides of the head that does not throb, is moderately intense, and is not made worse by physical activity. Additionally, these symptoms are experienced for 8 or more days a month for at least 3 months, or other headache symptoms are experienced that require the use of migraine-stopping medications.
- There may or may not be a long history of taking medications to relieve headaches (although it is more likely that chronic migraine has been caused by migraine that has progressed, especially when the migraine has not been treated effectively, than caused by overuse of medications).
Immediately seek medical attention if you or someone you are caring for experiences any of the following:
- Stiff neck and a high fever associated with headache
- Sudden onset of a severe headache
- Loss of motor function, the ability to think clearly, or convulsions associated with headache
- Head injury
- Increased intensity and/or frequency of headaches
Who's At Risk?
Those who suffer from chronic migraine usually have had migraines in the past with usual symptoms (nausea, vomiting, sensitivity to light and sound, headache that gets worse with activity. Chronic migraine is more common in women who have had migraine without what is known as visual aura. Visual aura is a problem with vision that leads in to the headache. There are many kinds of visual aura, but common experiences include floating lines, jagged shapes, flashing lights, or dark patches.
Usually, adults with chronic migraine have fewer “traditional” migraine attacks as part of their headache problem, while teenagers with chronic migraine are often bothered by the more traditional migraines as described above. Some reasons for getting chronic migraine include both too little treatment of migraine, and, conversely, too much treatment of migraine, particularly too much ibuprofen or medicines that contain caffeine. Other factors that can cause regular migraine to progress into chronic migraine are being overweight, too much stress, and snoring.
Signs & Symptoms
People who have migraine and develop chronic migraine notice a change in symptoms over months to years, during which normal migraine symptoms become less intense but the headaches become more frequent. Normal migraine symptoms can include headache as well as dark spots in vision, shimmering distortion at the edges of vision, dizziness, problems concentrating, trouble finding words, weakness, numbness, or tingling. Daily or almost daily headaches that resemble tension-type headaches develop that include pain on both sides of the head that does not throb, is moderately intense, and is not made worse by physical activity. In this new type of headache, now called chronic migraine, full migraines still occur in addition to the milder but daily headaches.
Self-Care Guidelines
Please see Common and Classical Migraine via the VisualDx Disease List for self-care ideas to help with traditional migraine symptoms. Some things you can do specific to the chronic migraine aspect of this type of headache are to avoid over-the-counter medications and caffeine because part of the problem can be overuse of these medicines (also see Medication Overuse Headache). More often, the chronic migraine is thought to be a progression of “traditional” migraines that have been undertreated. Therefore, paying very close attention to your normal migraine treatment can be helpful. Joining a discussion group, either in person or online, can give you some ideas and support for managing the pain. Some things you can do include:
- Improve sleep habits
- Regular exercise
- Yoga or stretching
- Massage therapy
- Relaxation techniques or exercises
Treatments
It can take a long time, sometimes years, before you and your doctor(s) can break the cycle of chronic migraine. Many things in a person’s daily regimen and lifestyle can influence and maintain chronic migraine. You and your doctor will want to look into:
- Anxiety and depression.
- Frustration.
- Physical and emotional dependence.
- Physical/lifestyle (eg, obesity, snoring, diet, poor sleep habits).
- Chronic medication overuse/misuse.
It is very important to have a clear idea of the plan and what to expect in order to get chronic migraine under control. Patience and working closely with your doctor are both very important. The worst part for some people is that headache often gets worse with treatment and lifestyle changes before it gets better. Strategies employ management of other conditions that may play a role in worsening migraine while medication detoxification, if applicable, is ongoing. Possibilities for management and prevention of headache include:
- Formal referral for relaxation therapies/hypnosis/biofeedback.
- Referral to a sleep expert.
- Cognitive-behavioral therapy – talk therapy with a trained counselor to help identify stressors and develop coping strategies to minimize symptoms.
- Counseling and treatment for depression and/or anxiety.
Medicines that you may use include standard migraine-preventative agents such as blood pressure medicines like beta-blockers (propranolol, atenolol) or clonidine, anticonvulsants (valproic acid, topiramate), tricyclic antidepressants (amitriptyline), calcium channel blockers (verapamil), and selective serotonin uptake inhibitors (fluoxetine, sertraline, paroxetine). Most are started at a low dose and gradually increased until the daily headache is better, and then these are often eventually tapered off themselves. In some cases in order to break the cycle of pain, you may have to stop all pain medications and start over. Several medications can be used to control the pain when you have stopped all others, including oral corticosteroids that are tapered (prednisone or dexamethasone for 3–7 days), or a short course of regular around-the-clock triptan therapy. These medications act as a “bridge” to a more normal routine once the daily pain is controlled. For difficult headache syndromes, hospitalization for intravenous dihydroergotamine (DHE) or Thorazine and diphenhydramine may be necessary for effective detoxification. Consulting with your doctor is necessary to determine which strategy is best for you.
Visit Urgency
People with chronic migraine often come to neurologists or headache specialty clinics because they notice that their headaches are more frequent, even if milder, and that their usual migraines are continuing. However, call your doctor right away for any headache if:
- You develop new symptoms not typical of prior headaches.
- An unusually severe headache occurs.
- You pass out or lose time.
- Your headache lasts an unusually long time.
- Headache awakens you from sleep.
- Fever and neck pain or stiffness are present.
Last modified on October 6th, 2022 at 3:06 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder