Basal Cell Carcinoma (BCC)
Basal cell carcinoma (BCC), also known as basal cell epithelioma, is the most common form of skin cancer. Basal cell carcinoma usually occurs on sun-damaged skin, especially in light-skinned individuals with a long history of chronic sun exposure. Although it requires treatment to prevent it from becoming too invasive, basal cell carcinoma does not typically metastasize, or spread to lymph nodes or internal organs.
There are several sub-types of basal cell carcinoma, including:
- Nodular BCC
- Infiltrating BCC
- Superficial BCC
Who's At Risk?
Although anyone of any ethnic background and any age can develop basal cell carcinoma, the overwhelming majority of people with this type of skin cancer are white and middle-aged or elderly. In fact, more than 99% of people with basal cell carcinoma are white, and more than 95% are between the ages of 40 and 80 years old. Men and women seem to develop basal cell carcinoma at fairly equivalent rates.
In addition, sun exposure plays a large role in the development of basal cell carcinoma. People who live in sunnier climates or who spend time outdoors due to work or hobbies are more likely to have basal cell carcinoma.
Signs & Symptoms
The most common location for basal cell carcinoma is on sun-damaged skin, especially the following areas:
- Face
- Head
- Neck
- Chest
- Upper back
However, basal cell carcinomas can occur on any part of the skin, except for the palms and soles.
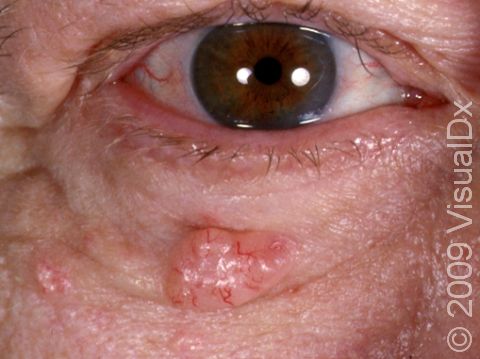
Nodular basal cell carcinomas are described as “pearly” in appearance. They are usually skin-colored or pink bumps, and tiny blood vessels (telangiectasias) can frequently be seen on their surfaces. As a basal cell carcinoma grows, it can develop a shallow depression in its center, and bleeding with minor trauma can occur.
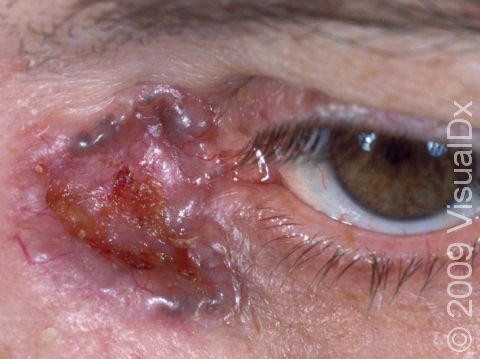
Infiltrating BCCs tend to appear as scar-like growths on the skin. They can be slightly shiny, and sometimes have telangiectasias, sores (erosions), or scabs on their surfaces. These skin changes can be subtle.
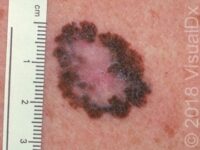
Superficial BCCs often appear as pink or red dry, scaly spots. They slowly enlarge and may develop a raised edge. Often, people mistake a superficial BCC as a dry patch of skin or a non-itching rash that won’t go away. This subtype of BCC is most often found on the trunk (chest or upper back), arms, or legs.
Self-Care Guidelines
Preventing sun damage is crucial to avoiding the development of a basal cell carcinoma. Wearing a broad-spectrum sunscreen with SPF 30 or higher and donning wide-brimmed hats and long-sleeved shirts can help avoid some sun exposure. In addition, staying out of the sun in the middle of the day (between 10:00 AM and 3:00 PM) can be helpful.
If you suspect that you may have a basal cell carcinoma, you should see your primary care provider or a dermatologist as soon as possible. There are no effective self-care treatment options.
Once a month, you should perform a self-exam to look for signs of skin cancer. It is best to perform the exam in a well-lit area after a shower or bath. Use a full-length mirror with the added assistance of a hand mirror when necessary. Using a hair dryer can help you examine any areas of skin covered by hair, such as your scalp.
- In front of a full-length mirror, inspect the front of your body making sure to look at the front of your neck, chest (including under breasts), legs, and genitals.
- With your arms raised, inspect both sides of your body making sure to examine your underarms.
- With your elbows bent, examine the front and back of your arms as well as your elbows, hands, fingers, area between your fingers, and fingernails.
- Inspect the tops and bottoms of your feet, the area between your toes, and toenails.
- With your back to the mirror and holding a hand mirror, inspect the back of your body, including the back of your neck, shoulders, legs, and buttocks.
- Using a hand mirror, examine your scalp and face.
As you perform your monthly self-exam, familiarize yourself with the moles, freckles, and other marks on your body, and look for any changes in them from month to month, including shape, size, color, or other changes, such as bleeding or itching.
Treatments
If your physician suspects a basal cell carcinoma, he or she will first want to establish the correct diagnosis by performing a biopsy of the lesion. The procedure involves:
- Numbing the skin with an injectable anesthetic.
- Sampling a small piece of skin by using a flexible razor blade, a scalpel, or a tiny cookie cutter (called a “punch biopsy”). If a punch biopsy is taken, stitches (sutures) may be placed and will need to be removed 6–14 days later.
- Having the skin sample examined under the microscope by a specially trained physician (dermatopathologist).
Treatment of a biopsy-proven basal cell carcinoma depends upon many factors, including the subtype of basal cell carcinoma, its size, its location on the face or body, and the general health of the patient.
Nodular basal cell carcinomas:
- Freezing (cryosurgery) with liquid nitrogen – Very cold liquid nitrogen is sprayed onto the basal cell carcinoma, freezing it and destroying it in the process.
- Electrodesiccation and curettage, also known as “scrape and burn” – After numbing the lesion, the doctor uses a curette to “scrape” the skin cancer cells away, followed by an electric needle to “burn,” or cauterize, the tissue. The electrodesiccation helps to kill the cancer cells and also to staunch any bleeding of the site.
- Excision – The basal cell carcinoma is cut out with a scalpel, and sutures are usually placed to bring the wound edges together.
- Mohs micrographic surgery – In this technique, the physician takes tiny slivers of skin from the cancer site until it is completely removed. This technique is particularly useful for basal cell carcinomas located on the nose, the ears, and the lips.
- Radiation treatment – X-ray therapy is often useful for patients who are not good surgical candidates because of other health issues.
Infiltrating basal cell carcinomas:
Infiltrating basal cell carcinomas can be more aggressive and locally destructive than other types of basal cell carcinoma. They can invade more deeply and widely than may first be evident by the superficial appearance of the skin cancer. For this reason, it is more important to treat them early and with slightly more aggressive techniques.
- Excision – The basal cell carcinoma is cut out with a scalpel, and sutures are usually placed to bring the wound edges together.
- Mohs micrographic surgery – In this technique, the physician takes tiny slivers of skin from the cancer site until it is completely removed. This technique is particularly useful for basal cell carcinomas located on the nose, the ears, and the lips.
- Radiation treatment – X-ray therapy is often useful for patients who are not good surgical candidates because of other health issues.
Superficial basal cell carcinomas:
Superficial basal cell carcinomas tend to be slow-growing and, as the name implies, very thin. Therefore, they do not necessarily need the more aggressive forms of treatment. In fact, some research indicates that superficial basal cell carcinomas may be treated without surgery.
- Cryosurgery with liquid nitrogen – Very cold liquid nitrogen is sprayed on the basal cell carcinoma, freezing it and destroying it in the process.
- Electrodesiccation and curettage, also known as “scrape and burn” – After numbing the lesion, the doctor uses a curette to “scrape” the skin cancer cells away, followed by an electric needle to “burn,” or cauterize, the tissue. The electrodesiccation helps to kill the cancer cells and also to staunch any bleeding of the site.
- Radiation treatment – X-ray therapy is often useful for patients who are not good surgical candidates because of other health issues.
- Imiquimod – This cream encourages the body’s immune system to attack and eradicate the superficial basal cell carcinoma. It is usually applied several times per week for 6–12 weeks.
- Photodynamic therapy – In this relatively new technique, a photosensitizing substance (a chemical that is activated when it is exposed to light) is applied to the superficial basal cell carcinoma. After an incubation period in which the chemical is preferentially absorbed by the skin cancer cells, the superficial basal cell carcinoma is exposed to a particular wavelength of light in the physician’s office. The special light activates the chemical, causing destruction of the superficial basal cell carcinoma.
- Laser – For superficial basal cell carcinomas, some physicians are using carbon dioxide and other lasers to destroy the skin cancer.
Visit Urgency
If you have developed a new bump on sun-exposed skin, or if you have a spot that bleeds easily or does not seem to be healing, then you should make an appointment with your primary care physician or with a dermatologist.
Try to remember to tell your doctor when you first noticed the lesion and what symptoms, if any, it may have (such as easy bleeding or itching). Also, be sure to ask your parents, siblings, and adult children whether or not they have ever been diagnosed with a skin cancer, and relay this information to your physician.
Trusted Links
References
Bolognia, Jean L., ed. Dermatology, pp.1672-1674, 1676-1693. New York: Mosby, 2003.
Freedberg, Irwin M., ed. Fitzpatrick’s Dermatology in General Medicine. 6th ed, pp. 747, 768. New York: McGraw-Hill, 2003.
Last modified on November 2nd, 2022 at 10:55 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder