Anthrax
Anthrax is a disease caused by the bacterium Bacillus anthracis, a bacterium that has the ability to form spores; spores are cells that are essentially dormant (asleep) but may become active under certain conditions. Anthrax disease can take 3 forms:
- Involving the skin (cutaneous) – 20% mortality
- Involving the lungs (inhalational) – 90% mortality
- Involving the digestive system (gastrointestinal) – 100% mortality
The vast majority of cases of anthrax (95%) are cutaneous. As a naturally occurring disease, anthrax is very rare. However, it has the potential to be used as a weapon of bioterrorism; this occurred in 2001 with an attack on the United States via the US Postal service. Anthrax was mixed in powder that was put into letters and packages and sent to prominent US figures, including senators. A number of people contracted cutaneous or inhalational anthrax from exposure to the powder, and some people died. If there were to be future attacks on the US using anthrax, it would probably be disseminated as an aerosol, and the resulting cases would be inhalational anthrax.
Who's At Risk?
B. anthracis is a very rare bacterium, and it causes disease infrequently. It is present naturally in both wild and domestic animals and in soil, particularly where an infected animal has died or been killed. People in contact with infected animals are at higher risk of contracting anthrax; these people include:
- Veterinarians
- Meat processors
- Animal shearers
- Tanners
In the case of a bioterrorism attack, anyone exposed to B. anthracis is at risk of contracting anthrax. Other people at high risk include:
- Postal workers
- Lab workers in facilities with B. anthracis
- Scientists studying B. anthracis
Signs & Symptoms
Cutaneous Anthrax
- Characteristic rash*
*The characteristic rash of anthrax looks like pink, itchy bumps that occur at the site where B. anthracis comes into contact with scratched or otherwise open skin. The pink bumps progress to blisters, which further progress to open sores with a black base (called an eschar). The early rash (the pink, itchy bumps) looks like many other rashes, so a history of exposure to the bacterium will be important to making the diagnosis. The eschar is more characteristic of anthrax infection, but if diagnosis and treatment are delayed until the eschar appears, the prognosis is poor.
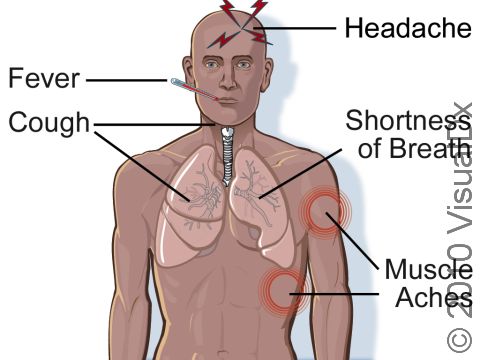
Inhalational Anthrax
Early symptoms:
- Cold or flu-like illness
- Fever
- Aches
- Sore throat
Later symptoms:
- Cough
- Chest pain
- Shortness of breath
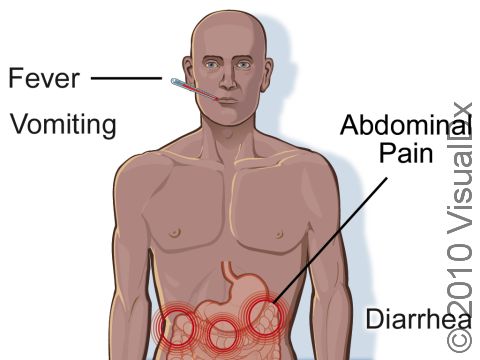
Gastrointestinal Anthrax
- Fever
- Nausea
- Decreased appetite
- Diarrhea, usually bloody
- Abdominal pain
Self-Care Guidelines
As with any illness, take care to rest and stay well hydrated when infected with anthrax. If you have open wounds, keep them clean and covered. Caretakers and household members should note that anthrax is not known to be contagious person to person.
Treatments
Your doctor can diagnose anthrax by testing your blood, respiratory secretions, or wounds. The diagnosis may be difficult to make without history of exposure, so be sure to tell your doctor if you think you may have come into contact with B. anthracis or if you meet any of the above risk factors.
Anthrax is treated with common antibiotics. If you have been exposed but are not yet sick, you will get the anthrax vaccine. (This vaccine is available only to people in the military, people who work with B. anthracis, and people who have been exposed to B. anthracis.) If you are infected, you will take a long course of antibiotics.
Visit Urgency
Seek care early if you think you have been exposed to B. anthracis. Treatment is more effective the earlier it is begun.
Trusted Links
Last modified on October 5th, 2022 at 7:01 pm

Not sure what to look for?
Try our new Rash and Skin Condition Finder