Acne Keloidalis Nuchae
Acne keloidalis nuchae, also known as folliculitis keloidalis, is a chronic skin condition characterized by inflamed papules (small, solid bumps), pustules (small, pus-filled bumps), and scars on the back of the neck.
Although it is not related to common acne, acne keloidalis nuchae initially appears as acne-like lesions of inflamed hair follicles on the back of the neck, and without treatment, it can result in small or large keloid-like scars and potentially hair loss in the affected area.
Who's At Risk?
Acne keloidalis nuchae can affect any race / ethnicity, but it is most commonly found in young adult Black men or, less commonly, Latino and Asian men. It is very uncommon in women. In addition, acne keloidalis nuchae is very rarely seen in people before puberty or after middle age.
Signs & Symptoms
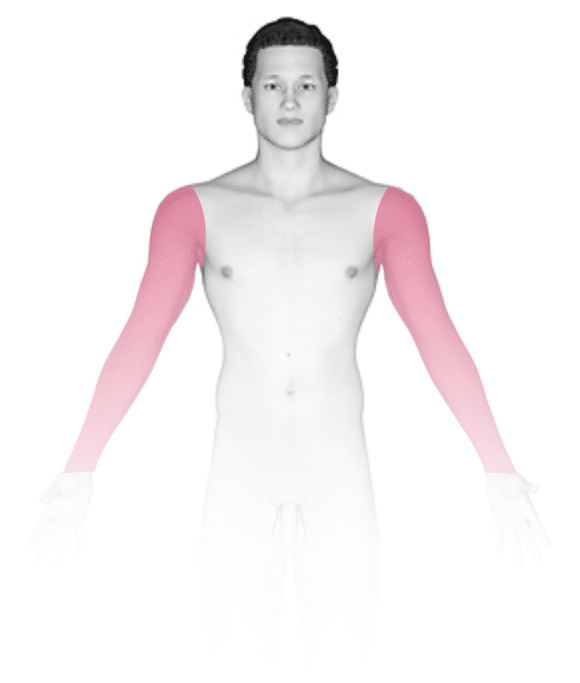
The most common locations of acne keloidalis nuchae include the:
- Back of the neck (posterior neck).
- Back of the scalp (occipital scalp).
Early on, lesions of acne keloidalis nuchae appear as inflamed or pus-filled bumps (papules and pustules), which may be painful and itchy. In darker skin colors, the lesions may be pink, reddish, or any shade of brown, whereas in lighter skin colors, they are pink or red. Over time, these inflamed bumps develop into small, raised scars. Without treatment, the small scars can form into large, thick scars. Areas of widespread scarring may be associated with hair loss. Sometimes advanced acne keloidalis nuchae lesions can develop deep pockets of pus (sinuses) with connections to the surface of the skin, and a foul-smelling discharge may ooze from these sinus tracts.
Self-Care Guidelines
Individuals with acne keloidalis nuchae should focus on avoiding irritation to the area to help prevent the formation of additional lesions, including:
- Washing the area gently with nonirritating cleansers. (Avoid scrubbing.)
- Avoiding wearing headwear (such as sports helmets) and shirt collars that rub against the back of the neck.
- Avoiding closely shaving the back of the scalp and neck.
For itchy lesions, try an over-the-counter hydrocortisone (eg, Cortisone) cream.
Although these self-care measures can help, anyone with acne keloidalis nuchae should see a health professional for treatment in order to prevent progression of the condition.
Treatments
Treatment for acne keloidalis nuchae is most effective when started early.
Topical creams, lotions, or gels may include:
- A retinoid cream such as tretinoin (Retin-A), tazarotene (Avage, Tazorac), or adapalene (Differin).
- A prescription-strength steroid or cortisone preparation.
- A topical antibiotic such as clindamycin (Cleocin T).
Oral medications may include:
- Antibiotic pills such as mupirocin (Bactroban, Centany), doxycycline (Doryx, Adoxa), or rifampin (Rifadin).
- A short course of steroids, such as prednisone (Delatsone, Rayos), for severe or advanced cases only.
Procedures to reduce inflammation and reduce or remove scar tissue include:
- Steroid injections directly into the inflamed bumps or scars.
- Surgical removal of single bumps or larger scars.
- Laser therapy / destruction.
- Liquid nitrogen (freezing or cryotherapy).
Visit Urgency
If you suspect you have acne keloidalis nuchae, you should seek help from a health professional such as a dermatologist to prevent the possible formation of large scars and permanent hair loss to the involved areas.
Trusted Links
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
James WD, Elston D, Treat JR, Rosenbach MA. Andrew’s Diseases of the Skin. 13th ed. Philadelphia, PA: Elsevier; 2019.
Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology. 9th ed. New York, NY: McGraw-Hill Education; 2019.
Last modified on March 31st, 2023 at 1:49 pm
Not sure what to look for?
Try our new Rash and Skin Condition Finder








